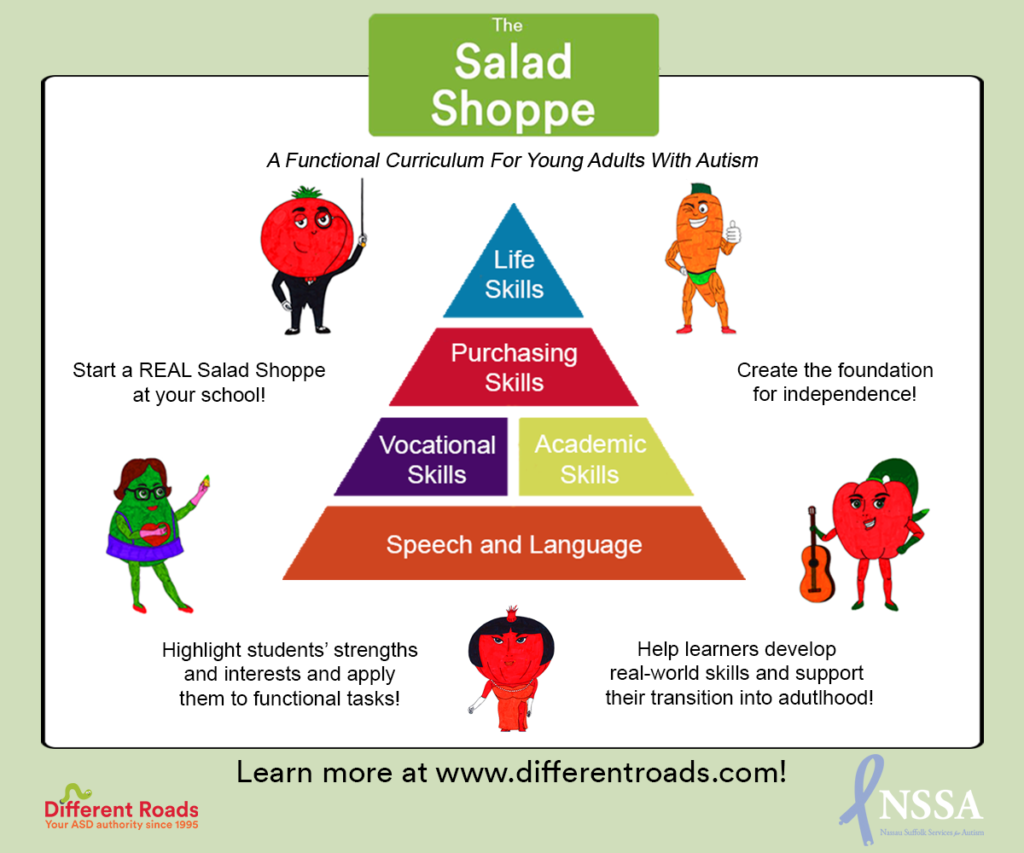
This week, save 15% on our brand new vocational curriculum! Click on the graphic for more details!
This month’s ASAT feature comes to us from Peggy Halliday, MEd, BCBA. To learn more about ASAT, please visit their website at www.asatonline.org. You can also sign up for ASAT’s free newsletter, Science in Autism Treatment, and like them on Facebook!
The following websites include milestones’ checklists, booklets, and a wealth of information to help parents become savvy consumers of autism treatment. The contributors are parent groups well as professional, medical, scientific, and legal and/or advocacy organizations which are available to meet the needs of families.
American Academy of Pediatrics (AAP)
The AAP is an organization of 67,000 pediatricians committed to the well-being of infants, children, adolescents, and young adults. The AAP website contains recent information about autism prevalence, links to many external resources and training websites, information about pediatrician surveillance and screening, and early intervention guidelines. This site offers great tools and resources for both pediatricians and families.
Association for Behavior Analysis International (ABAI)
The ABAI is a nonprofit professional membership organization whose objective for education is to develop, improve, and disseminate best practices in the recruitment, training, and professional development of behavior analysts. ABAI offers membership to professionals and consumers, which entitles them to a newsletter and other benefits, including event registration discounts, and continuing education opportunities.
Association of Professional Behavior Analysts (APBA)
The APBA is a nonprofit professional membership organization that is focused on serving professional practitioners of behavior analysis by promoting and advancing the science-based practice of applied behavior analysis. Membership is open to professional behavior analysts and others who are interested in the practice of ABA, including professionals from various disciplines, consumers, and students.
Association for Science in Autism Treatment (ASAT)
The ASAT is a non-profit organization founded in 1998 “to promote safe, effective, science-based treatments for people with autism by disseminating accurate, timely, and scientifically sound information, advocating for the use of scientific methods to guide treatment, and combating unsubstantiated, inaccurate and false information about autism and its treatment.” To serve its mission ASAT provides a comprehensive website which includes Research Synopses of a vast array of autism treatments to help families and organizations make informed choices, as well as specific resources for journalists, medical providers, and parents of newly diagnosed children. ASAT also publishes a monthly online publication, Science in Autism Treatment, with over 12,000 subscribers from all 50 states and over 100 countries. ASAT has Media Watch Initiative that responds quickly to both accurate and inaccurate portrayals of autism treatment in the media, and an Externship Program which includes students, professionals, and family members.
Autism NJ is now the largest statewide network of parents and professionals dedicated to improving the lives of individuals with autism and their families. Since its establishment in 1965, Autism New Jersey’s mission has been to ensure that all individuals with autism receive appropriate services. Autism New Jersey is a nonprofit agency committed to ensuring safe and fulfilling lives for individuals with autism, their families and the professionals who support them through awareness, credible information grounded in science, education, and public policy initiatives.
The Autism Science Foundation (ASF)
As well as providing information about autism to the general public and promoting awareness of the needs of individuals and families affected by autism, the Autism Science Foundation’s mission is to support and fund scientists and organizations conducting research into Autism Spectrum Disorder.
Autism Speaks supports global research into the causes, prevention, treatments, and cure for autism and raises public awareness. The website contains information on resources by state, resources for families, advocacy news, and suggested apps for learners with autism. The Autism Speaks 100 Day Kit for Newly Diagnosed Families of Young Children was created specifically for families of children ages 4 and younger to make the best possible use of the 100 days following their child’s diagnosis of autism.
Autism Wandering Awareness Alerts Response Education (AWAARE).
This organization has developed three “Big Red Safety Toolkits” to respond to wandering incidents: one for caregivers, one for First Responders, and one for teachers. They are free and downloadable from their website.
Behavior Analyst Certification Board (BACB)
The BACB is a nonprofit corporation established as a result of credentialing needs identified by behavior analysts, state governments, and consumers of behavior analysis services. Their mission is to develop, promote and implement an international certification program for behavior analysis practitioners. The BACB website contains information for consumers (including a description of behavior analysis), conduct guidelines, requirements for becoming certified and maintaining certification, and a registry of certificants that can be searched by name or state.
Cambridge Center for Behavioral Studies
The Cambridge Center for Behavioral Studies website seeks to bring together knowledge and behavior analysis resources, a glossary of behavioral terms, online tutorials and suggestions for effective parenting. A continuing education course series is offered through collaboration with the University of West Florida and is designed to provide instruction in a variety of areas of behavior analysis. To utilize all of the features of the website, you must register.
Centers for Disease Control and Prevention (CDC)
The Act Early website from the CDC contains an interactive and easy-to-use milestones’ checklist you can use to track how your child plays, learns, speaks, acts, and moves ages 3 months through 5 years. The milestones checklist is now available as a free downloadable tracker that follows your child’s progress. There are tips on how to share your concerns with your child’s doctor and free materials that you can order, including fact sheets, resource kits, and growth charts.
Council of Parent Attorneys and Advocates, Inc. (COPAA)
The Council of Parent Attorneys and Advocates is a national American advocacy association of parents of children with disabilities, their attorneys, advocates, and others who support the educational and civil rights of children with disabilities. The website provides important information about entitlements under federal law and is divided into resources for students and families, attorneys, advocates, and related professionals, and a peer to peer connection site.
Council for Exceptional Children (CEC)
The CEC is an international professional organization dedicated to improving the educational outcomes and quality of life for individuals with exceptionalities. The focus is on helping educators obtain the resources necessary for effective professional practice. Autism is one of many disabilities discussed.
Education Resources Information Center (ERIC)
Sponsored by the Institute of Education Services (IES) of the U.S. Dept. of Education, ERIC provides ready access to education literature to support the use of educational research and information to improve practice in learning, teaching, educational decision-making, and research.
The First Signs website contains a variety of helpful resources related to identifying and recognizing the first signs of autism spectrum disorder, and the screening and referral process. A video glossary is useful in demonstrating how you can spot the early red flags for autism by viewing side-by-side video clips of children with typical behaviors in comparison with children with autism. First Signs aims to lower the age at which children are identified with developmental delays and disorders through improved screening and referral practices.
Individuals with Disabilities Act (IDEA)
IDEA is a law that ensures services to children with disabilities throughout the nation. IDEA governs how states and public agencies provide early intervention, special education, and related services to more than 6.5 million eligible infants, toddlers, children, and youth with disabilities. The IDEA website contains information on early intervention services, local and state funding, and Individualized Educational Plan (IEP) issues including evaluation, reevaluation, and procedural safeguards.
The Interagency Autism Coordinating Committee (IACC)
IACC coordinates ASD related activities across the United States Health and Human Services Department and the Office of Autism Research. The IACC publishes yearly summary advance updates from the field of autism spectrum disorder.
The NAC is a nonprofit organization dedicated to disseminating evidence-based information about the treatment of autism spectrum disorder and promoting best practices. Through the multi-year National Standards Project, the NAC established a set of standards for effective, research-validated educational and behavioral interventions. The resulting National Standards Report offers comprehensive and reliable resources for families and practitioners.
National Professional Development Center on Autism Spectrum Disorders (NPDC)
In 2014 the NPDC, using rigorous criteria, classified 27 focused interventions as evidence- practices for teaching individuals with autism. This website allows you to access online modules for many of these practices as well as an overview and general description, step-by-step instructions, and an implementation checklist for each of the practices. NPDC is currently in the process of updating the systematic review through 2017 as part of the Clearinghouse on Autism Evidence and Practice. It also has a multi-university center dedicated to the promotion of evidence-based practices for ASD. The Center operates three sites at UC Davis MIND Institute, Waisman Center, and the Franklin Porter Graham Child Development Institute at the University of North Caroline Chapel Hill. Each of these websites delivers a wealth of information including online training modules, resources, factsheets, and more.
NIH National Institutes of Health (NIH)
The NIH, a part of the U.S. Department of Health and Human Services, is the primary federal agency for conducting and supporting medical research. Helping to lead the way toward important medical discoveries that improve people’s health and save lives, NIH scientists investigate ways to prevent disease as well as researching the causes, treatments, and even cures for common and rare diseases.
The Ohio Center for Autism and Low Incidence (OCALI)
OCALI working in collaboration with the Ohio Department of Education, is a clearinghouse of information on autism research, resources, and trends. The OCALI website contains training and technical assistance including assessment resources and ASD service guidelines.
Organization for Autism Research (OAR)
OAR is a nonprofit organization dedicated to applying research to the daily challenges of those living with autism. OAR funds new research and disseminates evidence-based information in a form clearly understandable to the non-scientific consumer. The OAR website contains downloadable comprehensive guidebooks, manuals, and booklets for families, professionals, and first responders. OAR offers recommendations and worksheets for educators and service providers to assist in classroom planning, and a newsletter, “The OARacle.” In conjunction with the American Legion Child Welfare Foundation, OAR also offers Operation Autism for Military Families, a web-based resource specifically designed and created to support military families that have children with autism.
Rethink is a global health technology company which provides cloud-based treatment too for individuals with developmental disabilities and their caregivers. Their web-based platform includes a comprehensive curriculum, hundreds of dynamic instructional videos of teaching interactions, step-by-step training modules, and progress tracking features.
Virginia Commonwealth University Autism Center for Excellence
VCU-ACE is a university-based technical assistance, professional development, and educational research center for autism spectrum disorder in the state of Virginia. VCU-ACE offers a wide variety of online training opportunities for professionals, families, individuals with ASD, and the community at large. The website contains many useful resources, including a series of short how- to videos demonstrating particular evidence-based strategies, webcasts, and online courses.
Wrights Law is an organization which provides helpful information about special education law, education law, and advocacy for children with disabilities in the USA. The Wrights Law website contains an advocacy and law library including articles, cases, FAQs and success stories, and information on IDEA.
Zero to Three: National Center for Infants, Toddlers, and Families
This is a national, nonprofit organization which seeks to inform, educate, and support professionals who influence the lives of infants and toddlers. The organization supports the healthy development and well-being of infants, toddlers, and their families by supplying parents with practical resources that help them connect positively with their babies. They also share information about the Military Families Project, which supplies trainings, information, and resources for military families with young children.
Please use the following format to cite this article:
Halliday, P. (2016 revised 2019). Consumer Corner: Some resources for parents. Science in Autism Treatment, 13(2), 27-31.
Peggy Halliday, MEd, BCBA, has served as a member of the Board of Directors of ASAT since 2010. She has been a practitioner at the Virginia Institute of Autism (VIA) in Charlottesville, Virginia since 1998. She oversees trainings for parents and professionals and provides consultation to public school divisions throughout Virginia.
For January, I have selected not one, but two texts. The first is a foundational article that every behavior analyst has probably read more than once. However it’s an important one to revisit, and one that I gain more insight from with each read. The second is a follow-up to the original article.
Article One: Baer, D. M., Wolf, M. M., & Risley, T. R. (1968). Some current dimensions of applied behavior analysis. Journal of Applied Behavior Analysis, 1(1), 91-97.
Article Two: Baer, D. M., Wolf, M. M., & Risley, T. R. (1987). Some still‐current dimensions of applied behavior analysis. Journal of Applied Behavior Analysis, 20(4), 313-327.
Discussion Questions for Baer, Wolf, Risley (1968):
The tone of the 1968 article is hopeful. The authors express a belief that behavior analytic procedures will become more prevalent as people understand the technology. Do you think they were accurate in this belief? What has been your experience with people accepting the principles of ABA?
Among the seven dimensions discussed in this article, what did you find most interesting?
The authors state that the term applied is defined by the interest society shows in the problem being studied. Is this how you have thought of the term applied in the past? How does your current work fit into this description? And how do we know society is interested?
In their discussion of analytic, the authors explain two designs commonly used to demonstrate reliable control of behavior change. Do you use these designs in your every day practice? Why or why not?
Do you think all seven of these dimensions hold equal importance? Why or why not?
How do the seven dimensions make ABA different from other fields?
Discussion Questions for Baer, Wolf, Risley (1987):
Compare and contrast the descriptions of each of the seven dimensions across the two articles.
The authors identify social validity as a good measure of effectiveness. However, they also identify issues with the assessment of social validity. How do you think that has changed since they wrote this article? How do you assess social validity in your own work?
What do you think of the discussion of high-quality failures?
In what ways do you follow the seven dimensions in your current work?
Can you identify a way to improve your own work based on the seven dimensions?
If you were to identify an eighth dimension that is not currently represented in these articles, what might you add?
SAM BLANCO, PhD, LBA, BCBA is an ABA provider for students ages 3-15 in NYC. Working in education for twelve years with students with Autism Spectrum Disorders and other developmental delays, Sam utilizes strategies for achieving a multitude of academic, behavior, and social goals. She is also an assistant professor in the ABA program at The Sage Colleges.
This month’s ASAT feature comes to us from Dr. Daniel W. Mruzek, PhD, BCBA-D, Associate Professor, University of Rochester Medical Center. To learn more about ASAT, please visit their website at www.asatonline.org. You can also sign up for ASAT’s free newsletter, Science in Autism Treatment, and like them on Facebook!
Marketers of purported interventions for autism spectrum disorder (ASD), whether they are pills, devices, or exercises, claim that their products are effective. As proof, they point to any number of measures some valid, some questionable, and some potentially misleading. Given that many of these “treatments” may be costly, ineffective and even dangerous, it is good to consider what constitutes legitimate measures of therapeutic benefit. How will we know if the intervention actually works?
A first step when presented with a potential treatment option is to investigate its scientific record. One can certainly ask the marketer (or therapist, interventionist, clinician, etc.) for examples of peer-reviewed studies examining the effectiveness of their recommended intervention. Indeed, this can be a great first step. An honest marketer will be glad to give you what they have in this regard or freely disclose that none exist. A good second step is to consult with a trusted professional (e.g., physician, psychologist, or behavior analyst who knows your family member), in order to get an objective appraisal of the intervention. If, after this first level of investigation is completed, a decision is made to pursue a particular intervention for a family member there are additional questions that one can ask the marketer prior to implementation that may prove very helpful in determining effectiveness after the intervention has been employed. These include the following:
Question 1: “What behaviors should change as a result of the intervention?”
Virtually any ASD intervention that is truly effective will result in observable change in behavior. For example, a speech intervention may very well result in increased spoken language (e.g., novel words, greater rate of utterances). An academic intervention should result in specific new academic skills (e.g., greater independent proficiency with particular math operations). An exercise purported to decrease the occurrence of challenging behavior will, if effective, result in a lower rate of specific challenging behaviors (e.g., tantrums, self-injury). As “consumers” of ASD interventions, you and your family member have every right to expect that the marketer will identify specific, objective, and measurable changes in behaviors that indicate treatment efficacy. Scientists refer to such definitions as “operational definitions” – these are definitions that are written using observable and measurable terms. If the marketer insists on using ill-defined, “fuzzy” descriptions of treatment benefit (e.g., “increased sense of well-being”, “greater focus and intentionality”, an increased “inner balance” or “regulation”), then “Buyer Beware!” These kinds of outcome goals will leave you guessing about treatment effect. Insist that operational definitions of target behaviors be agreed upon prior to start of intervention.
Question 2: “How will these behavior changes be measured?”
Behavior change is often gradual and variable. Behavior change often occurs in “fits and starts” (i.e., the change is variable). Also, our perception of behavior change can be impacted by any number of events (e.g., the co-occurrence of other therapies, our expectations for change). Therefore, it is the marketer’s responsibility to offer up a plan for collecting data regarding any change in the identified “target” behaviors. Usually, it is best to record numerical data (e.g., number of new words spoken by the individual, duration [in minutes] of tantrums, etc.) The use of numerical data to measure the change of operationally defined target behaviors is one of the best ways for a treatment team to elevate their discussion above opinion, conjecture and misrepresentation. If a pill, therapy or gadget is helpful, there is almost assuredly a change in behavior. And, that change is almost always quantifiable. Setting up a system to collect these numerical data prior to the initiation of the new intervention is a key to objective evaluation of intervention. Don’t do intervention without it.
Question 3: “When will we look at these intervention data and how will they be presented?”
Of course, it is not enough to collect data; these data need to be regularly reviewed by the team! One of the best ways to organize data is “graphically”, such as plotting points on a graph, so that they can be inspected visually. This gives the team a chance to monitor overall rates or levels of target behaviors, as well as identify possible trends (i.e., the “direction” of the data over time, such as decreasing or increasing rates) and look for change that may occur after the start of the new intervention. Note that the review of treatment data is generally a team process, meaning that relevant members of the team, including the clinicians (or educators), parents, the individual with ASD (as appropriate) often should look at these data together. Science is a communal process, and this is one of the things that makes it a powerful agent of change.
An interventionist with background in behavior analysis can set up strategies for evaluating a possible treatment effect. For example, in order to gage the effectiveness of a new intervention, a team may elect to use a “reversal design”, in which the target behaviors are monitored with and without the intervention in place. If, for example, a team wishes to assess the helpfulness of a weighted blanket in promoting a child’s healthful sleep through the night, data regarding duration of sleep and number of times out of bed might be looked at during a week with the blanket available at bedtime and week without the blanket available. Another strategy is to use the intervention on “odd” days and not use it on “even” days. Data from both “odd” and “even” days can be graphed for visual inspection, and, if the intervention is helpful, a “gap” will appear between the data sets representing the two conditions. These strategies are not complex, but they give the team an opportunity to objectively appraise whether or not a specific intervention is helpful that is much better than informal observation. Few things are as clarifying in a team discussion as plotted data placed on the table of a team meeting.
If the marketer does not answer these questions directly and satisfactorily, consider turning to a trusted professional (e.g., psychologist, physician or behavior analyst) for help. Families have a right to know whether their hard-earned money, as well as their time and energy, are being spent wisely. Asking these questions “up front” when confronted with a new intervention idea will help. Marketers have a responsibility to present their evidence – both the “state-of-the-science” as reflected in peer-reviewed research, as well as their plans to measure the potential effectiveness of their intervention for the individual whom they are serving.
Speaking of measuring treatment effectiveness, fellow ASAT board member Eric Larsson offers his considerations regarding the use of standardized measures (e.g., IQ) as outcome measures in treatment research (next article; page 20). Though this might be a little out of context for some of our readers, for those of us who rely on direct interpretations of peer-reviewed studies in our work (e.g., researchers, clinicians), Dr. Larsson describes the limitations of sole reliance on change in standardized measures is assessing the scientific validation of an intervention.
Please use the following format to cite this article:
Mruzek, D.W. (2014). ASD intervention: How do we measure effectiveness? Science in Autism Treatment, 11(3), 20-21
About The Author
Daniel W. Mruzek, Ph.D., BCBA-D is an Associate Professor at the University of Rochester Medical Center (URMC), Division of Neurodevelopmental and Behavioral Pediatrics in western New York. He received his doctoral training in Psychology at the Ohio State University and is a former Program Director at the Groden Center in Providence, Rhode Island. Currently, he is an associate professor and serves as a clinician and consultant, training school teams and supporting families of children with autism and other developmental disabilities.
Mruzek coordinates his division’s psychology postdoctoral fellowship program in developmental disabilities and is an adjunct faculty member in the University of Rochester Warner School of Education. He is actively involved as a researcher on several externally funded autism intervention research studies and has authored and co-authored more than 20 peer-reviewed articles and book chapters on autism and other developmental disabilities. Dr. Mruzek is on the editorial board for the journals Focus on Autism and Other Developmental Disabilities, Behavior Analysis in Practice, Journal of Mental Health Research in Developmental Disabilities, and Intellectual and Developmental Disabilities. Dr. Mruzek is a former member of the Board of Directors of the Association for Science in Autism Treatment.
The Salad Shoppe curriculum was developed by dedicated special educators who aspire to change the face of vocational training. Working with a group of 8 young adults with varying abilities, these teachers were charged with teaching academics and supporting their transition into adulthood.
This curriculum has changed the landscape of job training by highlighting the strengths and interests of each learner and applying them to functional tasks. The Salad Shoppe curriculum is a tool to take traditional teaching methods out of the classroom and integrate them into a comprehensive and functional setting.
I love token systems and use them frequently with my clients. Sometimes I use Velcro stars or stickers, or the Token Towers (which are great because you can hear the token going in the plastic tube.) It’s easy to vary the token system to fit the interests and age of a client I am working with. However, I see several errors in their use. Below are a few of the common ones:
• Inconsistent Use – The use of a token system should be predictable. When I am doing an ABA session, the token system is usually available throughout the session. But token systems may be specific to certain activities or certain environments. Using them only some of the time though doesn’t improve their effectiveness.
• Lack of Clarity – You should know what behavior you are focusing on for the token system. For example, I will write down for myself that I am providing tokens for a few specific behaviors (such as whenever a client responds correctly to a current learning target, when they remain in their seats for a period of five minutes, and when they greet a person who comes into the room.) It should be clear for you, as the person implementing the token system, what behaviors you are attempting to increase so you can provide tokens when those behaviors are exhibited.
• Lack of Differentiation – One of the things I love about token systems is that it allows me to easily differentiate reinforcement. For example, let’s say I’m working with a child to teach them to name items from different categories. Usually, when I ask them to name an animal, they name one animal and I provide a token for a correct response. But on this particular day, they name three animals. I can provide more than one token for the higher quality response.
• Not Allowing the Token System to Grow with the Child – Another benefit of token systems is that they can grow with the child. Once a child has mastered a certain behavior, I no longer include it in the token system. The child is always earning tokens for behaviors or responses that are difficult. If you have a client who has been receiving tokens for the same behavior for several months, then one of the two things is happening: (1) the client has mastered the behavior and you aren’t providing reinforcement for more challenging behaviors OR (2) the client has not mastered the behavior and for some reason your token system is not working. Either way, a change needs to be made.
• Fail to Provide a Motivating Reward – I have had some experiences in which the token was supposedly reinforcing on its own. In rare cases, this might just work. However, the tokens should be used to earn a known reinforcer for that particular client.
• Fail to Provide Choices in Rewards – There’s a great body of research on how choice improves motivation. Unfortunately, many children with developmental disabilities have fewer choices in their day-to-day lives than their typically developing counterparts. Allowing your client to choose from a selection of activities or toys for reinforcement will likely improve the quality of your token system.
Sam is an ABA provider for students ages 3-15 in NYC. Working in education for twelve years with students with Autism Spectrum Disorders and other developmental delays, Sam utilizes strategies for achieving a multitude of academic, behavior, and social goals. She is also an assistant professor in the ABA program at The Sage Colleges.
There is a common misconception that individuals with special needs require a slower pace of instruction. While they may require a slower pace through a curriculum, this does not mean that individual lessons should be taught at a slower pace. In fact, slowing the pace of instruction not only wastes precious instructional time, it may increase the occurrence of problem behaviors.
Higbee (2009) writes that “appropriately paced instruction helps students to maintain attention to the instructor and instructional materials. Though student attention can be lost when instruction is happening too rapidly, it is most often lost when the pace of instruction is not rapid enough” (p. 20).
So how can you maintain a fast pace of instruction that is appropriate for your student? Here are some things to consider:
Higbee, T. (2009). Establishing the prerequisites for normal language. In R. A. Rehfeldt, Y. Barnes-Holmes, & S.C. Hayes (Eds.), Derived relational responding applications for learners with autism and other developmental disabilities: A progressive guide to change (7-24). Oakland, CA: New Harbinger Publications, Inc.
Sam is an ABA provider for students ages 3-15 in NYC. Working in education for twelve years with students with Autism Spectrum Disorders and other developmental delays, Sam utilizes strategies for achieving a multitude of academic, behavior, and social goals. She is also an assistant professor in the ABA program at The Sage Colleges.
Technology can be a great addition to an educational or behaviorally supportive program for individuals with autism. It may be used as a powerful reinforcer for some, can facilitate language and communication, and help to organize and present visual and auditory cues efficiently. Items like tablets and smart phones also tend to be highly acceptable to learners, parents, and society as a whole. We have come a long way from the days of Velcro, laminate, and tackle boxes full of reinforcers! In some cases, the entire array of tools needed to support and teach may be included in a single device.
As great as technology may be for learners with autism, their families, and their teachers, however, there are some cautions that need to be observed. Here are some suggestions to make sure that technology is used effectively and does not have any detrimental effects.
1. Do carefully evaluate the functionality of the technology for the individual. Like any behavioral intervention, technology is not one-size-fits-all, and may not be appropriate for every use for every learner. Choose the type and application of technology that works best for the individual. Collect data on the success of the technology intervention, and make adjustments as needed.
2. Do teach alternative strategies that don’t rely on technology, to prepare for times when technology may be unavailable, broken, or inappropriate. Practice occasionally not using technology, so that when the inevitable happens (e.g., power outage, broken tablet, etc.), the individual is prepared and has some coping strategies.
3. Do monitor for safety and appropriate usage. Many apps are so easy for learners to use that they can easily connect with other people, make purchases, or share personal information without parents or teachers noticing. Devices that connect to the internet via wi-fi or data plans must be carefully monitored for such activity.
4. Do teach learners to manage their devices independently. Learners should know how to charge devices, set alarms and reminders, and use other apps for self-management. Technology isn’t just for fun; it’s become a part of life for most of us, and learners can benefit the same as anyone else.
5. Don’t use technology for technology’s sake. If it doesn’t serve a real purpose for teaching or behavioral support, it should not be in use. Any application of technology in teaching or behavioral interventions should be clearly defined, conceptually systematic, and precisely planned.
About The Author
Dana Reinecke, PhD, BCBA-D is a doctoral level Board-Certified Behavior Analyst (BCBA-D) and a New York State Licensed Behavior Analyst (LBA). Dana is a Core Faculty member in the Applied Behavior Analysis department at Capella University. She is also co-owner of SupervisorABA, an online platform for BACB supervision curriculum, forms, and hours tracking. Dana provides training and consultation to school districts, private schools, agencies, and families for individuals with disabilities. She has presented original research and workshops on the treatment of autism and applications of ABA at regional, national, and international conferences. She has published her research in peer-reviewed journals, written chapters in published books, and co-edited books on ABA and autism. Current areas of research include use of technology to support students with and without disabilities, self-management training of college students with disabilities, and online teaching strategies for effective college and graduate education. Dana is actively involved in the New York State Association for Behavior Analysis (NYSABA), and is currently serving as President (2017-2018).
There are many things that I would love to change about the treatment of individuals with Autism Spectrum Disorder. One of them is the notion that all kids with ASD are motivated by the same things. Certainly, some kids with autism love light up toys, squeezes, or music, but that’s true of the population at large. After all, I am mesmerized by Christmas lights, love a good head massage, and have songs I listen to on repeat.
The issue with the assumption that all kids with ASD are motivated by these small number of things is that it can lead to some very specific problems, such as practitioners trying out a smaller number of toys or activities with the child, practitioners depending solely on “sensory toys” for reinforcers instead of working to expand the number of reinforcers a child responds to, or the larger community making assumptions about the preferences of the child. Furthermore, there is evidence that the broader the range of reinforcers is for a child, the better the learning outcomes (Klintwall & Eikeseth, 2012.) Failing to think beyond the stereotypes about the interests of kids with ASD impedes their ability to learn and develop new skills.
The children I’ve worked with over the years have varied interests, ranging from dinosaurs and maps to bean bag toss and board games. And while some of the kids I work with love light up toys or trains, it’s important that we don’t take a whole swath of the population and decide that they all have similar interests. It doesn’t serve their skill development or our potential to develop real relationships with people with ASD.
As a practitioner, here are some important questions to ask yourself in relation to reinforcers and developing interests:
• Have you conducted a preference assessment? This should be one of the first things you do whenever you start a new case, and something you should continue to do informally.
• Have you talked to the client and/or the parents about what interests they would like to develop? If the client is able to discuss goals and interests with you, you should definitely be having that conversation with them. You should also talk to the parents about their goals. Perhaps they have seen some interest in one area that they would like to further develop. It’s also possible that there are specific family activities or traditions they would like their child to enjoy with the family.
• Have you read about this topic? A great place to start is Chapter 3 of the book A Work in Progress. It clearly explains how to use reinforcers and expand the reinforcer repertoire. There is also a ton of research out there about reinforcement. Take the time to search journals such as Journal of Applied Behavior Analysis and Journal of Developmental Disabilities.
Klintwall, L., & Eikeseth, S. (2012). Number and controllability of reinforcers as predictors of individual outcome for children with autism receiving early and intensive behavioral intervention: A preliminary study. Research in Autism Spectrum Disorders, 6(1), 493-499.
McEachin, J. & Leaf, R. B. (1999). A work in progress: Behavior management strategies and a curriculum for intensive behavioral treatment of autism. New York: DRL Books.
Sam is an ABA provider for students ages 3-15 in NYC. Working in education for twelve years with students with Autism Spectrum Disorders and other developmental delays, Sam utilizes strategies for achieving a multitude of academic, behavior, and social goals. She is also an assistant professor in the ABA program at The Sage Colleges.
The Discriminative Stimulus is defined as a stimulus in the presence of which a particular response will be reinforced (Malott, 2007, Principles of Behavior).
SD is just ABA speak for the demand, instruction, or the event/stimulus that serves as a signal to someone that there is something they need to respond to. Now, that response can also include a non-response. Not responding is always a possible choice, that comes with its own possible consequences.
For example, if my cell phone rings and it is someone I do not want to talk to I have choices:
-answer the phone
-don’t answer the phone
The phone ringing is a SD because when it rings, there is a specific response that in the past has led me to contact different consequences. Some pleasant, and some not so pleasant.
When my cell phone rings, I am not confused about what I should do. I know what my choices are, and depending on who is calling (or if I recognize who is calling) I then make a choice based on my history of reinforcement with that person.
SD’s can vary in how they are delivered, the specific reinforcement that they make available, as well as the specific expected response.
In ABA therapy sessions, sometimes hundreds of SD’s can be delivered throughout the session, and each one of those SD’s has a specific expected response, as well as specific consequences available for each possible response.
The SD has an authority based on the history of consequences being delivered.
I’ll say that another way: Let’s say I state the SD “give me blue” to a child, and I then provide a consequence of playing on an iPad if the child gives me yellow. Assuming playing on the iPad is a reinforcer, over time I am going to see the child consistently respond to my SD by giving me yellow. Is yellow in this example actually correct? No. But it does not matter: I gave my SD, I followed the child’s response with a reinforcer, and I have super-glued this particular response to the SD.
And this explains why your kids don’t listen.
Reinforcement is like the most powerful superglue on the market. It binds things together, as can be seen in the example below:
(SD) “Clean up the toys” —-> (Response) child cleans up the toys —> (Consequence) “Thanks so much, you can go outside now”
Assuming in the above example that going outside is a reinforcer, over time the child will learn the expected response to the SD of “clean up the toys”, AND they will learn that good things happen after they demonstrate the expected response. In other words, you just taught your child that when they clean up their toys, they might get to go outside.
If I flip this scenario on its head, I can show you how SD’s (and their absolute authority) can sometimes cause you to teach things you did not mean to teach:
(SD) “Clean up your toys” —> (Response) child cries/child screams “no!”/child does not respond to the SD —> (Consequence) “Ugh! Fine, I’ll clean the toys up. Just go outside while I clean up this mess”
Assuming in the above example that going outside is a reinforcer, over time what will the child learn? A few things actually:
-child will learn that problem behavior or not responding is a response
-child will learn that escape/avoidance behaviors work
-child will learn that cleaning up the toys is not a requirement to be able to go outside
Did you mean to teach that? I am nearly positive you did not. Unfortunately, the absolute authority of the SD remains unmoved by the fact that you didn’t intend to teach new ways to avoid a demand.
Don’t freak out, there is a way to avoid this trap.
First, understand what Instructional Control is and how it can help you. I promise, it isn’t as scary as it sounds.
Second, see below for some common characteristics of successful SD’s. A successful SD helps your child learn in an effective manner WHAT to do, and WHY to do it (because good things might happen). Let the absolute authority of the SD work for you, and not against you.
The SD is precise: A precise SD includes only the language necessary for the individual to know what to do. Extra details, threats, or reminders are best left off the SD, particularly if the individual has communication deficits or is very young. Good example – “Get down”. Not-so-good-example – “Michael Benjamin Clark, you get down off that railing right now before you fall and break your neck”.
The SD is stated, not asked: Unless you are cool with the individual tossing you a “No/I don’t feel like it/I don’t want to”, then do not present the SD as a question. A question gives the option of refusal.
The SD allows for a brief time to begin to respond: Brief as in, a few seconds. I have been in this field a long time, and I have developed an internal countdown timer that kicks in when I give a SD. To help yourself learn this skill, when you give your child a demand silently count to 3. Or, you could subtly tap a finger against the inside of your palm 3 times. If you get to 3 and the individual has not at least started to respond, it is time to provide a consequence. Another completely personal reason why I like this “internal countdown” is because it helps parents not flood the child with SD’s. If you are busy counting in your head, you can’t rattle off 4 more demands, when the child hasn’t even responded to demand #1.
The SD is consistent: Especially if the child has communication deficits or is very young, avoid changing up the SD rapidly. This can possibly be confusing, and impede learning. Once your child is demonstrating they know how to respond to the SD, that is the point where you can start to change the language used, or not use language at all (such as pointing at a book on the floor to indicate the child needs to put the book away).
The SD consequence is consistent: The most critical point about understanding SD’s is that what follows the response equals learning. You are teaching your child how to respond to you based on what happens when they respond correctly, and what happens when they respond incorrectly. If you decide that the SD “Make your bed” means fluffing all the pillows, then the bed being made with 1 pillow fluffed, or the bed being made with some of the pillows fluffed, are both incorrect responses. No exceptions. You would then prompt the correct response so the child knows they made an error.
Attention is gained before the SD is given: If you observe the ABA team work with your child you will get to see possibly hundreds of SD’s delivered during a therapy session. You may also note that the team works to gain the child’s attention before stating the SD, to make sure it is heard. This could look like approaching the child, bending/squatting down to look in the child’s face, waiting for a break in crying/screaming, or making a statement such as “Are you ready?”, to verify the child is attending.
The SD is not repeated over and over again, nor is it screamed, or shouted: SD’s are bosses. SD’s are in charge. SD’s call the shots. They do not need to beg, bargain, plead, scream, or lose their cool. Remember, your child only has a short time to respond correctly. If they do not respond correctly, you just deliver a consequence (such as a prompt). It will be very tempting to state the SD over and over again, but don’t give in to that temptation. Over time, this will actually teach your child they do not need to listen to you the first time, and that ignoring you is an effective way to avoid a demand.
About The Author
“I’ve been providing ABA therapy services to young children with Autism since early 2003. My career in ABA began when I stumbled upon a flyer on my college campus for what I assumed was a babysitting job. The job turned out to be an entry level ABA therapy position working with an adorable little boy with Autism. This would prove to be the unplanned beginning of a passionate career for me.
From those early days in the field, I am now an author, blogger, Consultant/Supervisor, and I regularly lead intensive training sessions for ABA staff and parents. If you are interested in my consultation services, or just have questions about the blog: contact me here.”
This piece originally appeared at www.iloveaba.com.