Teaching independent on-task behavior can be quite challenging when working with any student, but particularly so with some students with autism. In a study published in 2010, researchers Dina Boccuzzi Legge, Ruth M. DeBar & Sheila R. Alber-Morgan implemented and evaluated one way of teaching student to self-monitor their on-task behavior using a MotivAider. (The MotivAider is a simple electronic device that vibrates at timed intervals to provide an individual with a private prompt to engage in a specific behavior. It can be programmed to vibrate on a fixed or variable schedule at different duration and intensity levels.)
 In this study, the researchers worked with a fifth grader with autism, a sixth grader with autism, and a fifth grader with cerebral palsy. They taught the boys to wear the MotivAider (calling it a pager) and note a + or a – to indicate their behavior each time the MotivAider vibrated. The behaviors they monitored were all related to being on-task: “eyes on my work,” “in my seat,” and “doing work.” Once each boy consistently rated his behavior upon feeling the vibration, the researchers implemented the intervention.
In this study, the researchers worked with a fifth grader with autism, a sixth grader with autism, and a fifth grader with cerebral palsy. They taught the boys to wear the MotivAider (calling it a pager) and note a + or a – to indicate their behavior each time the MotivAider vibrated. The behaviors they monitored were all related to being on-task: “eyes on my work,” “in my seat,” and “doing work.” Once each boy consistently rated his behavior upon feeling the vibration, the researchers implemented the intervention.
The MotivAider’s were initially set to vibrate every two minutes. Each time the MotivAider vibrated, the student would mark a + or a – for each of the behaviors on a sheet he had on his desk. Prior to the intervention, the average percentages of time each boy was on-task ranged from 26% to 77%. Upon implementation of the intervention, “all three students showed an immediate and substantial increase of on-task behavior ranging consistently from 80% to 100%.
The researchers also included a plan for fading out the use of the MotivAider‘s, changing from a fixed schedule of every two minutes, to an increasing variable schedule. The fading schedules varied for each student. For example, for one student, the fading schedule started with a variable schedule of a vibration about every four minutes, then moved to about every six minutes, then to about every eight minutes, and then to about every ten minutes. The MotivAider was then removed completely.
After the intervention was complete, researchers collected data once a week for three weeks to see if the intervention was maintained. During all three maintenance probes, “all students continued to demonstrate 80%-100% on-task behavior.”
We’ve talked about how to use MotivAider‘s in the past, but I particularly love this intervention because it is feasible for teachers to implement in the classroom, promotes independence in learners with autism, and allows teachers to focus on other issues. Take a look at the study here to get a fuller description of how to implement such an intervention with your students.
For more information about the MotivAider, click here.
WRITTEN BY SAM BLANCO, MSED, BCBA
Sam is an ABA provider for students ages 3-12 in NYC. Working in education for ten years with students with Autism Spectrum Disorders and other developmental delays, Sam has developed strategies for achieving a multitude of academic, behavior, and social goals. Sam is currently pursuing her PhD in Applied Behavior Analysis at Endicott College.



 One quote from the paper states, “Not only do people strive for freedom in a broad sense they also enjoy making simple choices, such as whether to engage in unproductive, though harmless, activities, like watching sitcoms on television, eating too many doughnuts, taking time off from work, or taking a nap before dinner.” In an effort to teach our learners independent skills, we often neglect to teach meaningful decision-making that reflects the types of decisions neurotypical adults make every day. Since the paper was originally published, there has been more work done on promoting decision-making skills for learners with developmental disabilities, but the issues described in the paper are still relevant today.
One quote from the paper states, “Not only do people strive for freedom in a broad sense they also enjoy making simple choices, such as whether to engage in unproductive, though harmless, activities, like watching sitcoms on television, eating too many doughnuts, taking time off from work, or taking a nap before dinner.” In an effort to teach our learners independent skills, we often neglect to teach meaningful decision-making that reflects the types of decisions neurotypical adults make every day. Since the paper was originally published, there has been more work done on promoting decision-making skills for learners with developmental disabilities, but the issues described in the paper are still relevant today. When faced with feeding issues, many parents or caregivers may not consider seeking out help from a BCBA or behavior analyst. There is a tendency to associate ABA with sitting at a table and completing discrete trials, but this is only one tool in a behavior analyst’s extensive toolkit. Whether you are providing intervention for feeding issues or seeking more information, it is essential to look to scientific research for help.
When faced with feeding issues, many parents or caregivers may not consider seeking out help from a BCBA or behavior analyst. There is a tendency to associate ABA with sitting at a table and completing discrete trials, but this is only one tool in a behavior analyst’s extensive toolkit. Whether you are providing intervention for feeding issues or seeking more information, it is essential to look to scientific research for help.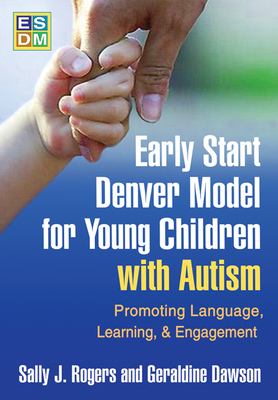 As the first comprehensive, empirically tested intervention specifically designed for toddlers and preschoolers with autism, the Early Start Denver Model (ESDM) is an early intervention approach for toddlers ages 12-36 months and continuing until ages 48-60 months. The model does not require a particular setting for implementation and can be used by parents, teachers, therapists, at home, in preschool or in a clinical setting. To help you get started with this early intervention model developed by Sally Rogers, Ph.D., and Geraldine Dawson, Ph.D., we are offering a 15% discount on the
As the first comprehensive, empirically tested intervention specifically designed for toddlers and preschoolers with autism, the Early Start Denver Model (ESDM) is an early intervention approach for toddlers ages 12-36 months and continuing until ages 48-60 months. The model does not require a particular setting for implementation and can be used by parents, teachers, therapists, at home, in preschool or in a clinical setting. To help you get started with this early intervention model developed by Sally Rogers, Ph.D., and Geraldine Dawson, Ph.D., we are offering a 15% discount on the 